
Perth researchers are planning to end the sleepless nights that families face when ear infections strike and won’t go away. Their research could reduce the need for antibiotics and surgery, and help tackle hearing loss in indigenous communities.
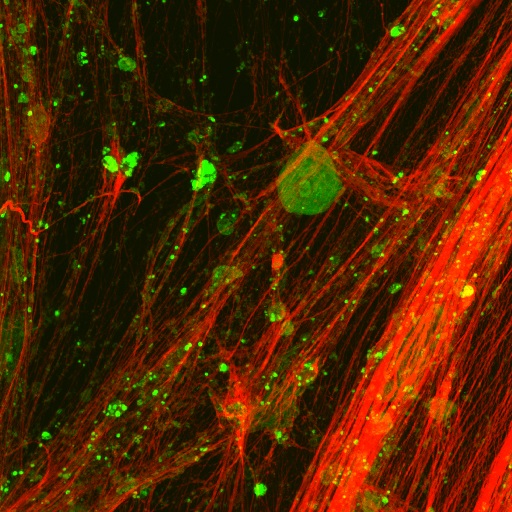
Dr Ruth Thornton and her research team at the University of Western Australia have discovered that sticky nets of DNA hide the bacteria in the ears of kids with recurrent middle-ear infections, where they evade antibiotic treatment by creating impenetrable slimy biofilms.
The researchers are targeting these nets with a drug that has already proven its ability to get kids with cystic fibrosis out of a sticky spot by breaking up thick secretions in their lungs. Clinical drug trials are currently underway and a study on the DNA net discovery was published in the online science journal Plos One in February.
“Bacteria in the ear hide in a sticky glue made up of big nets of DNA from the children’s own immune system. It is similar to what happens in the lungs of people with cystic fibrosis, where a treatment known as Dornase alfa is used to break this sticky DNA up,” said Dr Thornton, a research assistant professor in the school of paediatrics and child health.
“We are now trialling this treatment in the ears of children when they are having grommets put in. We believe this could get rid of these bacteria and stop children getting more infections and needing more ear surgery,” she said.
Middle ear infection, or otitis media, is one of the commonest childhood complaints. It occurs in the space behind the eardrum where fluid collects and bacteria can cause painful infections. For some children, this fluid doesn’t go away, becoming like egg white over time and leading to “glue ear”.
However, some children strike it extra unlucky with chronic infections that resist antibiotics and require the insertion of ventilation tubes, or grommets, in their eardrums. Thirty per cent of these children need repeat grommet surgery due to re-infection, and the condition’s chronic nature has been associated with hearing loss and learning difficulties.
The clinical trials at the University of Western Australia involve 60 children under the age of five, who will each receive dornase alfa in one ear during grommet surgery. The other ear will be used as a comparison and receive only surgery. Results will be collected over two years, with a larger national trial planned after this one is completed.
There are also plans to trial the treatment in indigenous children, who suffer from high rates of severe chronic middle ear infections, which can cause extensive hearing loss and chronically running ears.
“This is the first potential change in treating middle-ear infections for a long time, and more effective treatments will hopefully lead to improved hearing, better learning outcomes and a reduced burden on children and their families,” Dr Thornton said.
Ruth Thornton is one of 12 early-career scientists unveiling their research to the public for the first time thanks to Fresh Science, a national program sponsored by the Australian Government through the Inspiring Australia initiative.
For interviews:
• Niall Byrne, 0417 131 977, niall@scienceinpublic.com.au
University of Western Australia Media Manager:
• Sally-Ann Jones, 08 6488 3229








 Fresh Science is on hold for 2022. We will be back in 2023.
Fresh Science is on hold for 2022. We will be back in 2023.