A new diagnostic system used to detect cancer cells in small blood samples could next be turned towards filtering a patient’s entire system to remove those dangerous cells – like a dialysis machine for cancer – says an Australian researcher who helped develop the system.
The technique was developed for cancer diagnosis, and is capable of detecting (and removing) a tiny handful of cancer-spreading cells from amongst the billions of healthy cells in a small blood sample.
The revolutionary system, which works to diagnose cancer at a tenth of the cost of competing technologies, is now in clinical trials in the US, UK, Singapore and Australia, and is in the process of being commercialised by Clearbridge BioMedics PteLtd in Singapore.
“It’s like a non-invasive ‘liquid biopsy’ that can flag the presence of any type of solid cancer – like lung, breast, bowel, and so on – without the need for surgery,” says Dr Majid Warkiani, a lecturer at the School of Mechanical and Manufacturing Engineering at the University of New South Wales, and a project leader at the Australian Centre for NanoMedicine at UNSW.
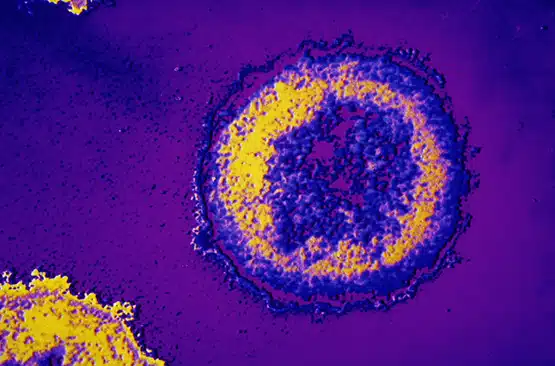
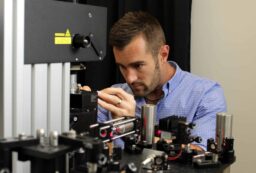
The initial challenge in developing the early-warning diagnosis system was to find those few cancer cells amongst billions of healthy blood cells. That challenge was met by a system that ‘spins out’ and isolates circulating tumour cells (CTCs), which are shed into the bloodstream from a solid tumour and can establish tumours elsewhere in the body—the mechanism by which cancer spreads through the body.
The ‘liquid biopsy’ can thus be used both for early cancer diagnosis and for monitoring a patient’s response to treatment.
But the potential for the new system goes far beyond just diagnosis.
If the filtering system could be scaled up, a cancer patient’s entire blood supply could potentially be similarly filtered, removing the dangerous cells and cycling the rest of the patient’s blood back into their system. It would be similar to dialysis treatment for kidney patients.
“It would be a revolution in cancer treatment. You would keep filtering out the dangerous cells, prolonging the life of the patient,” says Dr Warkiani. “There is still a long way to go—including securing money and support in Australia—before this is possible.’
But he believes this new technology will become one of the essential components of routine cancer management in the near future.
“A therapeutic version of this system, used for blood cleansing, could make the cancer a chronic disease and decrease drastically its mortality rate,” he says.
Majid was the NSW winner of Fresh Science, a national program that helps early-career researchers find and share their stories of discovery. Fresh Science is helping to build a cadre of skilled science communicators. In 2015, Fresh Science ran in every mainland state, with 180 early-career researchers nominating for the six Fresh Science events held this year in Melbourne, Townsville, Brisbane, Perth, Adelaide and Sydney.
Over 50 early-career researchers nominated for Fresh Science NSW, which was held at the Australian Museum (training) and Three Wise Monkeys Hotel (public challenge event) and was supported by the Australian Museum and the University of New South Wales.
For interviews:
Majid Warkiani (University of New South Wales) +61 424 100 396; m.warkiani@unsw.edu.au
Errol Hunt (Science in Public) +61 423 139 210; errol@scienceinpublic.com.au
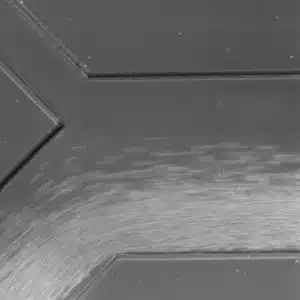
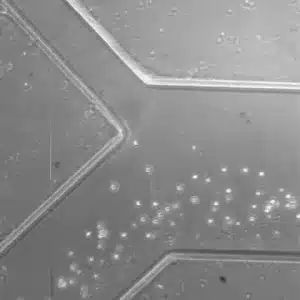
Isolation of cancer cells from normal blood cells (cancer cells go up). Warkiani Lab and ClearbridgeBioMedics Pte Ltd.
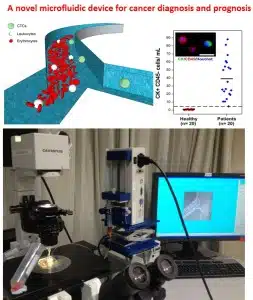
(Top): Schematic showing working mechanism of the newly developed microfluidic system for isolation of CTCs from blood. (Bottom): Image of the microfluidic system in operation
Isolation of Circulating Tumour Cells from a lung cancer patient (AVI)








 Fresh Science is on hold for 2022. We will be back in 2023.
Fresh Science is on hold for 2022. We will be back in 2023.